Neuropathy and Myopathy (न्यूरोपैथी एवं मायोपैथी)
Neuropathy and myopathy are distinct conditions affecting the neuromuscular system—neuropathy involves nerve damage, while myopathy affects muscle fibers directly. Both can cause weakness, pain, and functional impairment, but understanding their differences is crucial for proper diagnosis and treatment. With over 11 years of neurological experience, I’m here to explain these conditions clearly and compassionately.
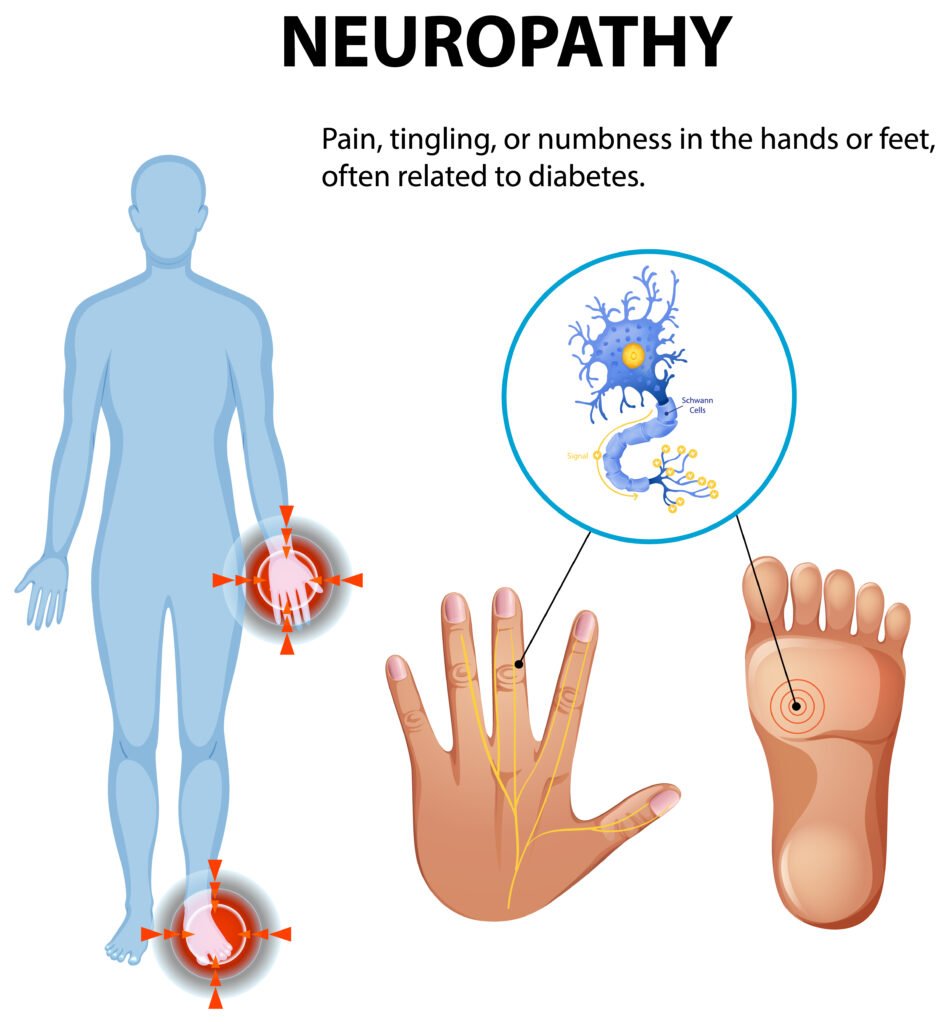
What Is Neuropathy?
Peripheral neuropathy occurs when nerves outside the brain and spinal cord are damaged, disrupting communication between the central nervous system and the rest of the body. This condition affects 20-30 million Americans and can involve:
Sensory nerves: Causing numbness, tingling, or burning pain
Motor nerves: Leading to muscle weakness and coordination problems
Autonomic nerves: Affecting heart rate, digestion, and blood pressure regulation
Common causes include diabetes (the leading cause), vitamin deficiencies, autoimmune conditions, infections, and certain medications.
What Is Myopathy?
Myopathy refers to diseases of muscle tissue where the primary problem lies within the muscle fibers themselves. Unlike neuropathy, the nerves remain intact, but the muscles cannot function properly. The National Institute of Neurological Disorders categorizes myopathies into several types:
Inflammatory myopathies: Including polymyositis and dermatomyositis
Inherited myopathies: Such as muscular dystrophies
Metabolic myopathies: Affecting energy production in muscles
Drug-induced myopathies: From medications like statins or steroids
Recognizing the Symptoms
Neuropathy Signs
Gradual onset of numbness or tingling in hands and feet
Sharp, stabbing, or burning pain
Muscle weakness, especially in distal muscles (hands and feet)
Loss of reflexes and coordination
Extreme sensitivity to touch
Myopathy Signs
Muscle weakness typically affecting proximal muscles (shoulders, hips, thighs)
Muscle pain or tenderness
Difficulty climbing stairs, rising from chairs, or lifting objects overhead
Muscle cramps or stiffness
In severe cases, breathing or swallowing difficulties
How We Diagnose
Clinical Assessment: Detailed history and physical examination to distinguish between nerve and muscle involvement.
Electrophysiological Studies:
Nerve Conduction Studies: Measure nerve signal transmission
Electromyography (EMG): Assesses muscle electrical activity
Laboratory Tests: Blood work for diabetes, vitamin levels, inflammatory markers, and muscle enzymes (CK, aldolase).
Imaging & Biopsy: MRI of muscles or nerve biopsy in selected cases.
For comprehensive diagnostic approaches, see the Mayo Clinic’s peripheral neuropathy guide.
Treatment Strategies
Neuropathy Management
1. Addressing Underlying Causes
Optimal diabetes control to prevent further nerve damage
Vitamin supplementation for deficiencies (especially B12, folate, thiamine)
Treatment of autoimmune conditions with immunosuppressants
2. Symptom Relief
Current treatment guidelines recommend:
First-line medications: Gabapentin, pregabalin, duloxetine, or amitriptyline
Topical treatments: Lidocaine patches or capsaicin cream for localized pain
Physical therapy: To maintain strength and prevent falls
Myopathy Treatment
1. Inflammatory Myopathies
Corticosteroids: Prednisone as initial therapy
Immunosuppressants: Methotrexate, azathioprine, or mycophenolate for steroid-sparing effects
Intravenous immunoglobulin (IVIG): For refractory cases
2. Supportive Care
Physiotherapy: Strengthening exercises and range-of-motion activities
Occupational therapy: Adaptive equipment and energy conservation techniques
Respiratory monitoring: For conditions affecting breathing muscles
Living Well with Neuropathy or Myopathy
Maintain regular exercise within your capabilities—swimming and gentle stretching are often beneficial.
Use protective footwear and check feet daily if you have diabetic neuropathy.
Practice fall prevention with proper lighting, handrails, and removal of trip hazards.
Monitor for medication side effects and maintain regular follow-up appointments.
Join support groups to connect with others facing similar challenges.
When to Reach Out
Seek evaluation if you experience:
Progressive muscle weakness or unexplained pain
Numbness or tingling that spreads or worsens
Difficulty with daily activities like walking, climbing stairs, or using your hands
Breathing or swallowing difficulties
Early diagnosis and treatment can slow progression and improve quality of life.
To schedule your personalized consultation:
Visit our Home Page
Together, we’ll develop a comprehensive treatment plan tailored to your specific condition—combining expert medical care with compassionate support.
—Dr. Rohit Anand
Consultant Neurologist, Jamshedpur