Sciatica / Slipped Disc (सायटिका / स्लिप डिस्क)
Sciatica and slipped (herniated) discs are common spine-related conditions that cause pain, numbness, or weakness radiating from the lower back into the buttocks and legs. Drawing on over 11 years of neurology expertise, I’ll explain their causes, evaluation, and effective treatments to help you regain comfort and mobility.
What Is Sciatica?
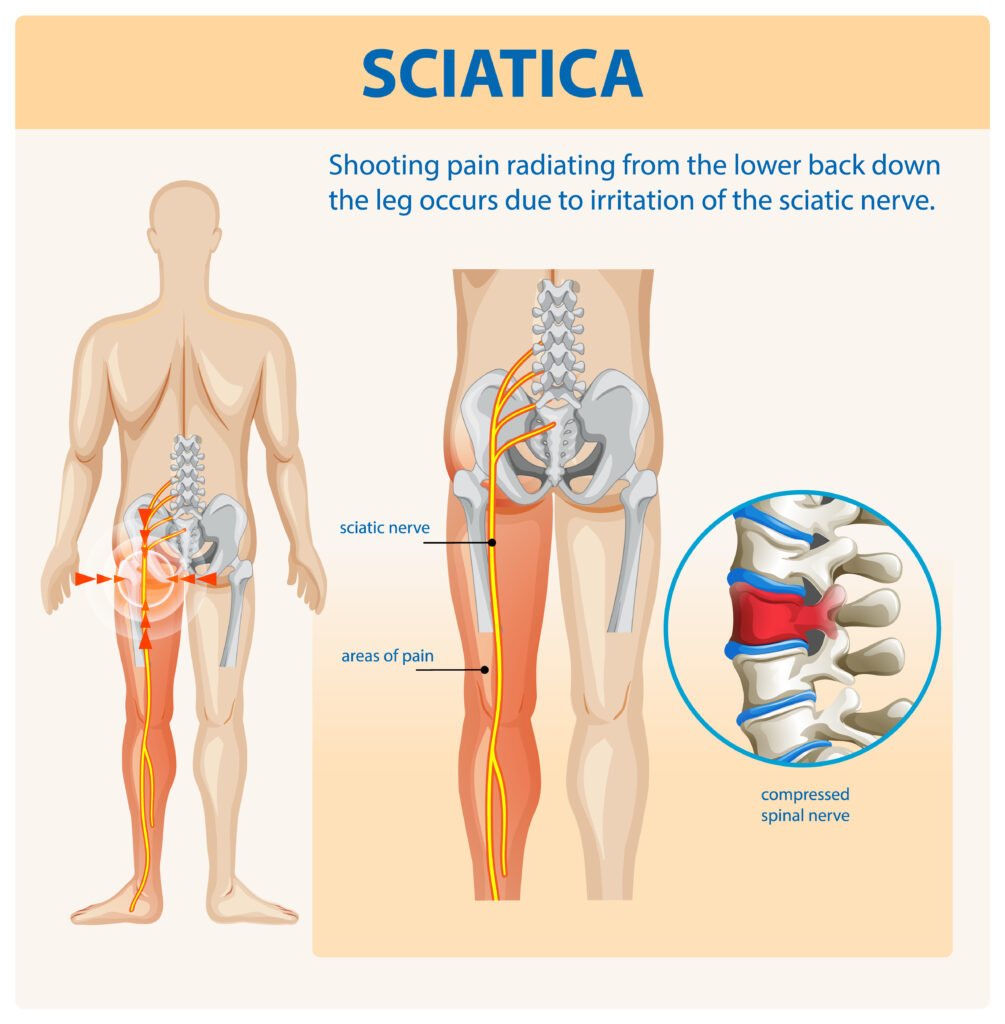
Sciatica refers to irritation or compression of the sciatic nerve, the largest nerve in the body, which runs from the lower spine through the buttocks and down each leg. Symptoms often include:
Sharp, shooting pain radiating down the leg
Numbness, tingling, or “pins and needles” in the foot or toes
Muscle weakness in the affected leg
Worsening pain when sitting, coughing, or sneezing
What Is a Slipped (Herniated) Disc?
Between each vertebra of your spine lies a gel-filled cushion called an intervertebral disc. When the outer ring (annulus fibrosus) weakens or tears, the inner nucleus can bulge or herniate, pressing on nearby nerves—often triggering sciatica. For an in-depth overview, see the Mayo Clinic’s guide to herniated discs.
Common Causes & Risk Factors
Age-related wear and tear (disc degeneration)
Heavy lifting or twisting with improper technique
Obesity, increasing spinal load
Sedentary lifestyle and poor posture
Smoking, which reduces disc oxygenation and healing
How We Diagnose
Clinical Evaluation: Detailed history of pain radiation, aggravating factors, and functional limitations.
Physical Exam: Assessment of reflexes, muscle strength, and straight-leg-raise test for sciatica.
Imaging Studies:
MRI to visualize disc herniation and nerve compression
CT or X-ray to rule out fractures and spinal alignment issues
Electrophysiological Tests: EMG and nerve conduction studies if diagnosis remains unclear.
Treatment Options
1. Conservative Care
Most patients improve with non-surgical measures over 4–6 weeks:
Activity Modification: Short rest followed by gradual return to light activities
Physical Therapy: Core-strengthening, stretching, and postural exercises
Medications: NSAIDs, acetaminophen, or short-term muscle relaxants
Epidural Steroid Injections: For persistent radicular pain
2. Advanced Interventions
If symptoms persist beyond 6–8 weeks or if severe weakness occurs, consider:
Minimally Invasive Discectomy: Removal of herniated disc material to decompress nerves
Microdiscectomy: Microsurgical technique with smaller incisions and faster recovery
Percutaneous Procedures: Such as nucleoplasty for contained herniations
Guidelines from the National Institute for Health and Care Excellence (NICE) recommend a stepped approach—prioritizing conservative care before surgery. For details, see NICE’s recommendations on low back pain and sciatica.
Preventing Recurrence
Practice proper lifting techniques: Bend at knees, keep objects close to your body.
Maintain core strength through regular exercise and Pilates or yoga.
Ensure an ergonomic workstation with lumbar support and frequent breaks.
Maintain a healthy weight and quit smoking to support disc health.
When to Seek Help
Contact a specialist if you experience:
Progressive leg weakness or foot drop
Loss of bladder or bowel control
Severe, unrelenting pain unresponsive to conservative care
New or worsening neurological symptoms
Early intervention can prevent complications and restore function.
To schedule your personalized evaluation:
Visit our Home Page
Together, we’ll develop a targeted treatment plan combining the latest evidence-based therapies with compassionate support—helping you overcome sciatica and slipped disc symptoms and return to the activities you love.
—Dr. Rohit Anand
Consultant Neurologist, Jamshedpur