Stroke (मस्तिष्क आघात)
A stroke occurs when blood flow to a part of the brain is interrupted—either by a clot (ischemic stroke) or by a burst blood vessel (hemorrhagic stroke)—leading to sudden loss of brain function. With over 11 years in neurology practice, I’ve seen how rapid recognition and treatment save lives and improve recovery. This guide explains stroke warning signs, evaluation, and management in clear, compassionate terms.
Recognizing Stroke Warning Signs
Remember the acronym BE FAST:
Balance loss or sudden dizziness
Eyesight changes—trouble seeing in one or both eyes
Face drooping—one side of the face may droop or feel numb
Arm weakness—one arm drifts downward when raised
Speech difficulty—slurred or strange speech
Time to call emergency services immediately
Time is brain: every minute counts. For more on stroke symptoms, see the American Stroke Association’s BE FAST guide.
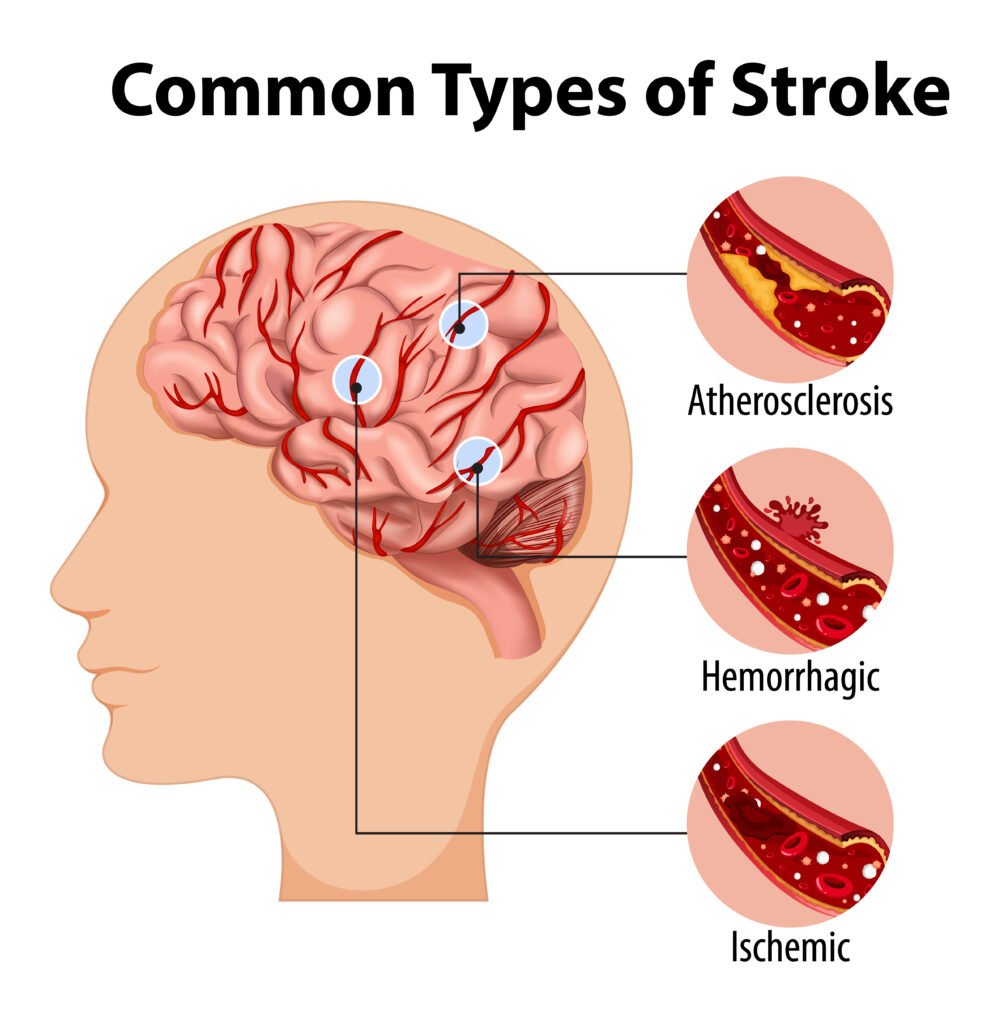
Types of Stroke
Ischemic Stroke (≈85%): Caused by a blood clot blocking a cerebral artery.
Hemorrhagic Stroke: Occurs when a blood vessel ruptures, leading to bleeding in or around the brain.
Transient Ischemic Attack (TIA): “Mini-stroke” with temporary symptoms—often a warning sign of future strokes.
How We Diagnose Stroke
Clinical Assessment: Immediate evaluation of vital signs, neurological deficits, and medical history.
Neuroimaging:
CT Scan rules out hemorrhage and guides urgent treatment.
MRI detects early ischemic changes and smaller infarcts.
Vascular Studies: Ultrasound or CT angiography to identify artery blockages or aneurysms.
Cardiac Evaluation: ECG and echocardiogram to detect heart rhythm disorders or source of emboli.
Acute Treatment
Ischemic Stroke
Thrombolysis: Intravenous tissue plasminogen activator (tPA) dissolves clots if given within 4.5 hours of symptom onset.
Mechanical Thrombectomy: Catheter-based clot removal within 6–24 hours for large-vessel occlusions.
Hemorrhagic Stroke
Blood Pressure Control: Aggressive management to limit bleeding.
Surgical Intervention: Clot removal or aneurysm repair when indicated.
Reversal of Anticoagulation: Urgent correction if patient was on blood thinners.
For detailed acute care protocols, refer to the National Institutes of Health’s stroke treatment guidelines.
Rehabilitation & Recovery
Stroke recovery is a journey requiring a multidisciplinary team:
Physiotherapy to rebuild strength and mobility.
Occupational Therapy to regain daily living skills.
Speech Therapy for language, swallowing, and cognitive challenges.
Emotional Support: Counseling and support groups to address mood changes and caregiver stress.
Preventing Recurrent Stroke
Blood Pressure Control: The single most effective measure.
Antiplatelet or Anticoagulant Therapy: Depending on stroke subtype.
Cholesterol Management: Statins to stabilize arterial plaques.
Lifestyle Modifications: Healthy diet, regular exercise, smoking cessation, and moderation of alcohol intake.
Comprehensive prevention strategies are outlined in the World Health Organization’s stroke prevention fact sheet.
When to Reach Out
If you or a loved one experiences any BE FAST warning signs, call emergency services without delay. Early hospital evaluation and treatment dramatically improve outcomes.
To arrange a consultation or post-stroke follow-up:
Return to our Home Page
With prompt intervention, personalized rehabilitation, and vigilant prevention, we can minimize stroke’s impact and help you regain independence and quality of life.
—Dr. Rohit Anand
Consultant Neurologist, Jamshedpur